Low-Grade Serous Ovarian Cancer: Unraveling the Mystery and Finding Hope
July 9, 2024

Low-grade serous ovarian cancer (LGSOC) is a rare subtype of ovarian cancer that often gets overshadowed by its more well-known counterpart, high-grade serous ovarian cancer. But just because it’s rare doesn’t mean it’s not important.
It’s time we put LGSOC in the spotlight and arm ourselves with the knowledge to fight back. Because when it comes to ovarian cancer, information is our secret weapon, and we’re not afraid to use it.
What Is Low-Grade Serous Ovarian Cancer (LGSOC)?
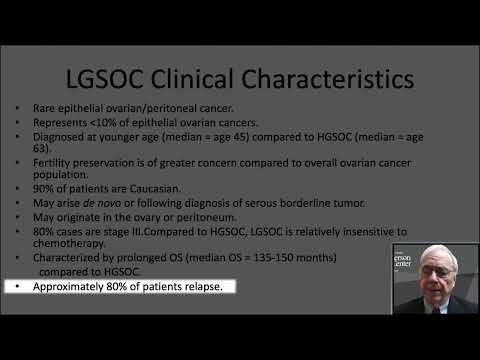
LGSOC (also known as low-grade serous carcinoma) is a type of epithelial ovarian cancer that accounts for less than 10% of all ovarian cancers. It’s a slow-growing kind of cancer that doesn’t get as much attention as its more aggressive high-grade counterpart. The cells in LGSOC look more like normal tissue, which sounds good, right? Well, not so fast. This sneaky characteristic actually makes LGSOC harder to detect early on.
Despite its slow growth, LGSOC can also be just as invasive as high-grade cancer, silently spreading to nearby organs. It’s a quiet threat that demands our attention and research efforts.
One thing to keep in mind is that LGSOC tends to affect younger women compared to high-grade serous ovarian cancer. According to ovarian cancer facts and research, the average age at diagnosis for LGSOC is around 45 years old, while for high-grade, it’s closer to 63. This means that LGSOC patients often face unique challenges, like balancing treatment with work, raising a family, managing fertility concerns, and dealing with early-onset menopause.
How Low-Grade Serous Ovarian Cancer Develops
Doctors, researchers, and scientists are still trying to piece together the puzzle of how LGSOC starts. It might come from the ovaries or the fallopian tubes. Some experts think it could develop step-by-step from borderline ovarian cancer or tumors (BOT), which are a type of ovarian tumor that’s not as invasive as traditional cancer. What we do know is that certain gene changes, like KRAS and BRAF mutations, are often found in LGSOC cells. These changes are like a secret code that sets LGSOC apart from other ovarian cancers.
But here’s the thing: not all LGSOC tumors have these mutations. Around 40% of LGSOC tumors don’t have any identifiable mutations at all. This makes studying LGSOC even more challenging, but also more critical. We need to figure out what makes these tumors tick so we can find better ways to treat them.
Low-Grade Serous Ovarian Cancer Symptoms
 LGSOC is notorious for flying under the radar. It’s often diagnosed at later stages when it has already spread beyond the ovaries.
LGSOC is notorious for flying under the radar. It’s often diagnosed at later stages when it has already spread beyond the ovaries.
The symptoms can be sneaky and mimic other common issues. Bloating, belly pain, feeling full quickly, and changes in peeing habits are all potential red flags. But here’s the thing: these symptoms can also show up in a myriad of other health conditions, from the most common gastrointestinal issues to cancer. That’s why it’s so hard to detect LGSOC with symptoms alone. You really have to listen to your body and advocate for yourself if something doesn’t feel right.
Some women with LGSOC also report other symptoms, like fatigue, back pain, constipation, and pain during sex. These symptoms can be easy to brush off or attribute to other causes, but if they persist or get worse, it’s always best to get them checked out.
Diagnosing Low-Grade Serous Ovarian Cancer
Diagnosing LGSOC is like solving a complex mystery. It takes a mix of different clues and tests. Imaging scans like ultrasounds, CT scans, and MRIs can give us a peek inside. The CA-125 blood test can also hint at ovarian cancer. This test measures the level of a protein called CA-125 (cancer antigen 125) in the blood. High levels can be a sign of ovarian cancer, but they can also be caused by other conditions, like endometriosis or fibroids.
Often, the definitive answer comes from a surgical biopsy, where doctors can examine the cells closely and determine whether it’s really LGSOC. During this procedure, the surgeon removes a small piece of tissue from the ovary or other suspicious areas. A pathologist then examines the cells under a microscope for the final diagnosis.
In some cases, doctors may also recommend somatic genetic testing to look for specific gene changes associated with LGSOC, like KRAS and BRAF mutations. This information can help guide ovarian cancer treatment decisions and give us a better understanding of the cancer’s behavior.
Differences Between Low-Grade and High-Grade Serous Ovarian Cancer
LGSOC and high-grade serous ovarian cancer (HGSOC) might sound similar, but their behaviors are very different. LGSOC cells are the slow-growing type, taking their time to spread. HGSOC cells, on the other hand, are more aggressive, multiplying and invading quickly.
The gene changes in these two cancers are also distinct. LGSOC often has KRAS and BRAF mutations, while HGSOC is known for BRCA and TP53 alterations.
The biggest difference is how they respond to treatment. LGSOC tends to be less sensitive to the usual chemotherapy drugs compared to HGSOC. While chemotherapy might knock out HGSOC, it often doesn’t pack the same punch against LGSOC. But don’t lose hope – this just means we need to get creative and find targeted, personalized treatments that work better for LGSOC.
Another key difference is survival rates. While HGSOC tends to grow and spread quickly, leading to poorer outcomes, LGSOC generally has a better prognosis. In one study, the median overall survival for advanced-stage LGSOC was 82 months, compared to 58 months for HGSOC. But it’s important to remember that every cancer is unique, and individual factors like age, overall health, and response to treatment can all impact survival.
Stages and Prognosis of Low-Grade Serous Ovarian Cancer
Like other ovarian cancers, LGSOC is staged from I to IV. Higher stages mean the cancer has spread further. The earlier LGSOC is caught, the better the chances of survival.
One study found that patients with stage II-IV LGSOC had a median overall survival of 82 months. That means half of the patients lived longer than 82 months. In contrast, patients with HGSOC had a median overall survival of 58 months. So, while LGSOC is no walk in the park, it generally has a better prognosis than its high-grade cousin.
But prognosis isn’t just about the numbers. Age, how much cancer is left after surgery, and the presence of certain gene changes can all impact survival. For example, being diagnosed at a younger age (35 or under) has been linked to worse outcomes in LGSOC. On the flip side, having MAPK gene changes has been tied to better overall survival in some studies.
It’s also worth noting that LGSOC tends to have a higher recurrence rate than HGSOC. In one study, over 70% of patients with advanced LGSOC experienced a recurrence at some point. But the good news is that recurrences are often slower-growing and more treatable than the initial cancer.
Low-Grade Ovarian Cancer Treatment Options
Surgery is the cornerstone when it comes to treating LGSOC. The goal is to remove as much of the visible tumor as possible. This could mean a major surgery to debulk the cancer, a fertility-saving surgery for younger patients, or a second surgery if the cancer comes back.
But surgery isn’t the only treatment option. Chemotherapy, while less effective in LGSOC compared to HGSOC, is still commonly used, despite its poor success rate. Many doctors still revert to it, but it really shouldn’t be used for LGSOC. Platinum-based chemo is also often used despite its extremely poor response rate.
Hormone therapy, especially with drugs called aromatase inhibitors, has shown some promise in LGSOC. These meds work by blocking estrogen, which can fuel the growth of LGSOC cells. In one study, the response rate to hormone therapy in recurrent LGSOC was around 9%, with 61% of patients achieving stable disease.
Targeted therapies, like MEK inhibitors and BRAF inhibitors, are the new kids on the block. They zero in on specific gene changes often found in LGSOC, like KRAS and BRAF. In a phase II study of the MEK inhibitor selumetinib, 15% of patients with recurrent LGSOC had an objective response, and 65% achieved stable disease.
Let’s not forget the importance of clinical trials. These are research studies testing new treatments and combinations to help improve outcomes and quality of life for LGSOC patients. Participating in a clinical trial gives you access to cutting-edge treatments and helps advance our understanding of LGSOC and how to treat it best.
Managing Recurrent Low-Grade Serous Ovarian Cancer
Recurrence is a common and frustrating part of the LGSOC journey. Unlike HGSOC, which often comes back within a couple of years, LGSOC can reappear many years after the first treatment. Studies show that over 70% of patients with advanced LGSOC will face a recurrence at some point.
But a recurrence doesn’t mean game over. There are lots of ways to manage LGSOC when it rears its ugly head again. A combination of systemic treatments prescribed by your doctor like chemo, hormone therapy, and targeted drugs can all be used. In some cases, a second surgery to remove the cancer might be an option.
Focusing on quality of life is just as important as fighting cancer. Palliative care is all about easing symptoms and improving overall well-being. It’s not just about living longer but living better. This can include things like pain management, counseling, and spiritual support.
It’s also important to have open and honest conversations with your ovarian cancer doctor and medical team about your goals and priorities. Some people may choose to focus on aggressive treatment, while others may prioritize quality of life over quantity. There’s no right or wrong answer; it’s all about what matters most to you.
Coping with a Low-Grade Serous Ovarian Cancer Diagnosis
Getting diagnosed with LGSOC can be a total gut punch. Fear, anger, sadness, uncertainty: it’s a whole mess of emotions. But you don’t have to deal with it alone. There are lots of support resources out there, like counseling, support groups, and online communities. Lean on them when you need to.
Talking openly with your medical team is also key. Don’t be afraid to ask questions, speak up about your worries, and fight for what you need. Your doctors and nurses are there to guide you, but you’re the boss of your own body.
For younger patients, fertility might be a big concern. Talking with your care team about options like fertility-saving surgery or freezing your eggs can help you make decisions about your future family plans. Some women may also choose to explore alternative paths to parenthood, like adoption or surrogacy.
Remember, you’re not alone in this. Connecting with other LGSOC patients and survivors can give you a sense of community and hope. Their stories can be a shining light on the darkest days. And if you’re feeling up to it, consider sharing your story. You never know who you might inspire or help along the way.
The Future of Low-Grade Serous Ovarian Cancer Research
The future of LGSOC research is full of possibilities. One of the benefits of ovarian cancer clinical trials is that they are the driving force behind finding new treatments and improving outcomes. When patients participate in these trials, they help researchers unlock the mysteries of LGSOC and find better ways to beat it.
Some exciting areas of study include finding new ovarian cancer biomarkers to help guide treatment decisions, developing new imaging techniques for earlier detection, and exploring combination therapies to boost treatment effectiveness.
But the most important part of LGSOC research is the shared goal of improving the lives of people affected by this disease. Every study, trial, and breakthrough is a step towards better outcomes, better quality of life, and, one day, a cure.
Of course, research takes money. That’s where organizations like Not These Ovaries come in. By donating to LGSOC research through our ovarian cancer research fund, you’re not just supporting scientific progress; you’re giving hope to the thousands of women and families affected by this disease. Every dollar counts, and together, we can make a real difference.
LGSOC may be a rare and challenging type of ovarian cancer, but it’s not unbeatable. With advances in research, personalized treatments, and a growing understanding of this tricky disease, we’re turning the tide in the fight against LGSOC.